Esophageal Cancer
Increase in obesity linked to rising numbers of esophageal cancer cases.
For most of his adult life, 49-year-old Jim Bonell suffered from acid reflux, but he never considered the condition dangerous. That is, until he was diagnosed with esophageal cancer.
What Bonell didn't know was that his chronic acid reflux left him with a condition called Barrett's esophagus, which puts people at high risk for esophageal cancer. Barrett's is a condition in which the cells lining the lower esophagus change because of repeated exposure to stomach acid. Normally, the tissue lining the esophagus is similar to the lining in your mouth (squamous mucosa), but with Barrett's, the body replaces the normal esophageal lining with one similar to that found in the intestines.
"There were no symptoms that I had esophageal cancer," says Bonell. "Prior to being diagnosed, my acid reflux was really bad and getting worse. I was a Tums-eater. I'd eat a whole bunch of them."
Esophageal cancer rates are on the rise, and the increase may be due to an increase in obesity, says Mark B. Orringer, M.D. professor and head of thoracic surgery at the University of Michigan Health System. Obesity often causes a hiatus hernia and associated acid reflux.
Esophageal cancer has always carried a terrible prognosis. But thanks to an increasing awareness that heartburn may have serious implications along with earlier detection, improved staging tests and better treatment many patients like Bonell are winning the battle with this initially "silent" cancer.
Bonell has benefited from some of the surgical advances developed and refined at the U-M Health System. Traditionally, patients who needed to have their esophagus removed–either for esophageal cancer or Barrett's esophagus – underwent highly invasive surgery that involved opening the chest and abdomen.
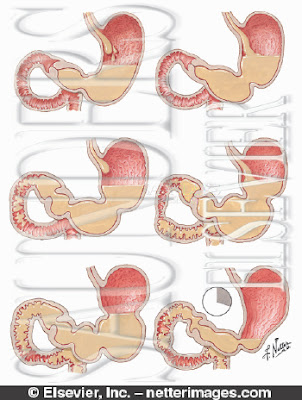
But Orringer and his colleagues developed a procedure, called transhiatal esophagectomy, in which the esophagus is removed through incisions in the abdomen and the neck, without the need to open the chest.
Once the esophagus is removed, the stomach is freed up from attachments holding it in the belly and it is pulled up through the chest. The stomach is then connected to the remaining esophagus in the neck.
The risk of infection is significantly lowered with this procedure because if any leak at the connection in the neck occurs, the resulting infection drains externally rather than in the chest, says Orringer. Further, by avoiding the traditional chest incision, pneumonia after this operation is much less common.
"In a recent study of more than 2,000 patients who have undergone a transhiatal esophagectomy at the University of Michigan, the hospital mortality rate in the last 1,000 patients was 1 percent; that's one death in 100 operations," he notes. "When I began as a faculty member in 1973, the mortality for esophagectomy was as high as 20 percent at many institutions."
This development in surgical treatment is important given the dramatic rise in cancer cases that doctors believe stems from obesity and acid reflux. Twenty years ago, the most common type of esophageal cancer was squamous cancer, which arises from the squamous mucosa that lines the normal esophagus.
But in the past 10 to 15 years, there has been a 350 percent increase in adenocarcinoma of the esophagus, a type of cancer that is related to the cellular changes in the esophagus that are the hallmark of Barrett's. It is now the most common form of esophageal cancer, occurring in 80 percent to 90 percent of patients. This increase in esophageal adenocarcinoma mirrors the rise of the obesity epidemic.
"There's no question that the incidence of esophageal cancer is increasing dramatically. We have an epidemic of obesity in this country," says Orringer. "I can't walk into a social setting where there are not some people who are quite overweight and complain of heartburn or acid indigestion. I think we should be very concerned."
Five tips for preventing Barrett's Esophagus and esophageal cancer
1. Work on losing weight. Obesity leads to hiatus hernia and reflux which are in turn responsible for the increasing rates of esophageal cancer. Talk to your family physician about developing a plan to lose weight by eating well and exercising regularly.
2. Don't lie down after eating. For those with acid reflux, the valve between the esophagus and the stomach doesn't function properly, allowing the contents of the stomach to back up into the esophagus. Lying down can make this problem worse, leading to late-night heartburn. Be sure to eat early to give your stomach time to empty before bedtime.
3. Sleep propped up. Lying down can exacerbate acid reflux. If you have reflux, consider arranging pillows so that your head and upper chest are elevated while you sleep. Stomach acid, like water, does not roll uphill.
4. Take an antacid. Neutralize stomach acid before it backs up into the esophagus with antacids.
5. Talk to your doctor. If you have a long history of severe heartburn or acid indigestion, talk to your doctor about Barrett's esophagus, which increases your risk of developing cancer. Even if your acid reflux symptoms are controlled, you still could be at risk. The only way to diagnose Barrett's is with an endoscopy and biopsy. Esophageal cancer can be cured, if it is diagnosed early.
 Focusing on 44 infants with ongoing spitting up or vomiting problems, researchers used a test to measure the reflux (or regurgitation) of acid from the stomach into the esophagus. What they found: The vast majority of the babies couldn't technically be diagnosed with gastroesophageal reflux disease (GERD), a condition that's different from regular old reflux. Reflux is very common in infants, but it usually doesn't cause any health problems and stops before a baby's first birthday. Doctors diagnose GERD when a child's reflux is causing complications, like irritation of the esophagus due to refluxed stomach acid, poor weight gain, or breathing problems due to spit up spilling over into the child's lungs.
Focusing on 44 infants with ongoing spitting up or vomiting problems, researchers used a test to measure the reflux (or regurgitation) of acid from the stomach into the esophagus. What they found: The vast majority of the babies couldn't technically be diagnosed with gastroesophageal reflux disease (GERD), a condition that's different from regular old reflux. Reflux is very common in infants, but it usually doesn't cause any health problems and stops before a baby's first birthday. Doctors diagnose GERD when a child's reflux is causing complications, like irritation of the esophagus due to refluxed stomach acid, poor weight gain, or breathing problems due to spit up spilling over into the child's lungs.